- By Talibuddin Khan
- Wed, 20 Apr 2022 10:14 AM (IST)
- Source:JND
New Delhi | Aalok Sensharma: Maternal mortality, the death of women during pregnancy or post-pregnancy, has been a key challenge for several countries around the globe, thanks to poor medical infrastructure and inadequate hospital staff to deal with such situations. In India, maternal health has been a key issue for successive governments since independence with the Maternal Mortality Ratio (MMR) being as high as 2,000 per one lakh live births in the 1940s.
In the 1950s, this came down to 1,000 and subsequently improved to 600 in the 1990s (at that time, the global MMR was 400), thanks to a rapid improvement in healthcare infrastructure, that rate has been reduced significantly.
Last month, the Union Health Ministry had said that India is on the verge of achieving the Sustainable Development Goals (SDGs) target of a Maternal Mortality Ratio (MMR) of 70 maternal deaths per lakh live births by 2030 as it noted that the Maternal Mortality Ratio has plunged by 10 points as per the Special Bulletin on MMR released by the Registrar General of India (RGI).
In a release, the ministry said there is a "progressive reduction" in MMR from 130 in 2014-2016 to 122 in 2015-17 to 113 in 2016-18, and 103 in 2017-19, adding that seven states have achieved the SDG target.

"Kerala (30), Maharashtra (38), Telangana (56), Tamil Nadu (58), Andhra Pradesh (58), Jharkhand (61), and Gujarat (70). There are now nine (9) States that have achieved the target of MMR set by the NHP which include the above 7 and the States of Karnataka (83) and Haryana (96)," the ministry said.

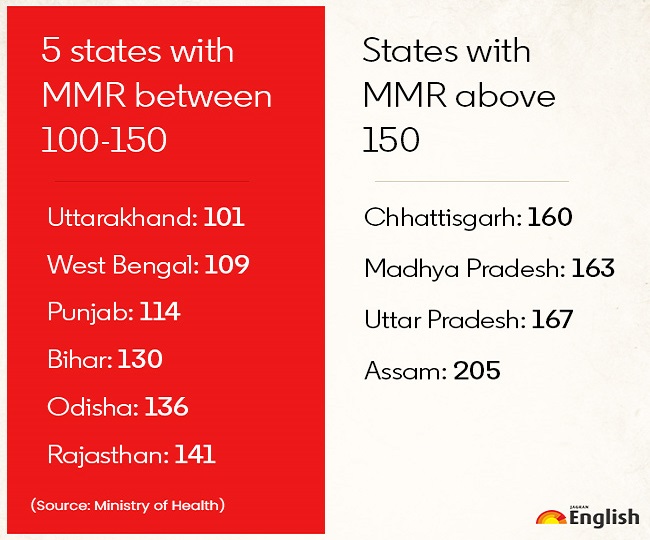
"Five states [Uttarakhand (101), West Bengal (109), Punjab (114), Bihar (130), Odisha (136) and Rajasthan (141)] have MMR in between 100-150, while for 4 states namely, Chhattisgarh (160), Madhya Pradesh (163), Uttar Pradesh (167) and Assam (205) have MMR above 150," it added.
Lauding the Uttar Pradesh government, it said the state has shown an "encouraging achievement" with a maximum decline of 30 points of MMR. However, it noted that four states - West Bengal, Haryana, Uttarakhand and Chhattisgarh - have shown an increase in MMR, asking them to reappraise their strategy.
"It is pertinent to point that strategic investments under National Health Mission (NHM) through various schemes have been consistently yielding increasing dividends," the Union Health Ministry said.
What is Maternal Mortality Ratio or MMR?
It is the number of maternal deaths during a given time period per 1 lakh live births. The MMR depicts "the risk of maternal death relative to the number of live births and essentially captures the risk of death in a single pregnancy or a single live birth".
"Maternal mortality is considered a key health indicator and the direct causes of maternal deaths are well known and largely preventable and treatable," says the United Nations International Children's Emergency Fund (UNICEF).
How is MMR calculated?
It can be calculated with the below-mentioned formula:
MMR = (Number of maternal deaths/ Number of live births) X 1,00,000
What does MMR signify about India?
Maternal health is an important factor in a country's development and the MMR is a key indicator that helps in determining the quality of health services of a nation. In India, the MMR was quite high in the 1990s with 600 women dying during childbirth per hundred thousand live births. At that time, the global MMR was 400, which means India was contributing to 27 per cent of the maternal deaths worldwide.
By 2010, the global MMR declined to 210. Likewise, it stood at 178 in India, a 70 per cent decline. By 2017-19, the MMR declined to 103, signifying the steps taken by the Centre to improve maternal health across the country.
"The Government of India has been focusing on initiatives to improve maternal health indicators. Much progress has been made in ending preventable maternal deaths in the past two decades: Globally the number of women and girls who die each year due to issues related to pregnancy and childbirth has dropped considerably, from 451,000 in 2000 to 295,000 in 2017, a 38 per cent decrease," said the WHO on its website.
Initiatives launched by the government to improve women and maternal health:
Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA): Launched by the Union Health Ministry in 2016, this scheme aims to provide pregnant women with fixed days, free of cost assured and quality Antenatal Care on the ninth day of every month.
Pradhan Mantri Matru Vandana Yojana (PMMVY): The scheme was originally launched in 2010, but renamed in 2017. Implemented by the Ministry of Women and Child Development, it is a direct benefit transfer (DBT) scheme under which cash benefits are provided to pregnant women in their bank accounts directly to meet enhanced nutritional needs and partially compensate for wage loss.
Labour Room Quality Improvement Initiative (LaQshya): Launched in 2017, it aims to improve the quality of care in the labour room and maternity operation theatres to ensure that pregnant women receive respectful and quality care during delivery and the immediate post-partum period.
POSHAN Abhiyaan: It is the Centre's overarching scheme for holistic nutrition. It aims to achieve improvement in the nutritional status of Children, Adolescent Girls, Pregnant Women and Lactating Mothers, in a time-bound manner.
Anemia Mukt Bharat (AMB): Launched by Union Health Ministry in 2018, it aims to reduce anaemia prevalence both due to nutritional and non-nutritional causes, in the lifecycle approach.
Surakshit Matratva Ashwasan (SUMAN): This scheme aims to provide assured, dignified, respectful and quality healthcare at no cost and with zero tolerance for denial of services for every woman and newborn visiting the public health facility to end all preventable maternal and newborn deaths.
Janani Suraksha Yojana (JSY): Launched in 2005, this scheme aims to reduce Maternal and Infant Mortality by promoting institutional delivery among pregnant women.
Janani Shishu Suraksha Karyakram (JSSK): This scheme aims to eliminate out-of-pocket expenses for pregnant women and sick infants by entitling them to free delivery including caesarean section, free transport, diagnostics, medicines, other consumables, diet and blood in public health institutions.